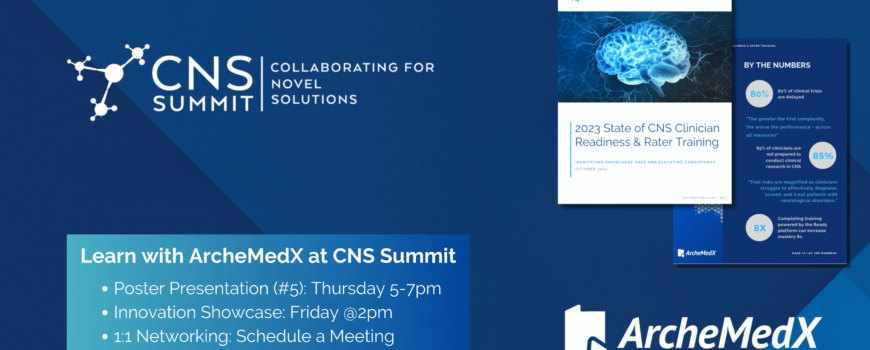
The Compounding Power of Training: Early Investment Yields Exponential Returns
The compounding benefits of effective training cannot be overstated. When clinical research associates (CRAs) and site staff are thoroughly prepared, they engage more deeply with the trial protocols, ask more insightful questions, and more proactively anticipate challenges.