Today’s New Reality in Clinical Trial Readiness
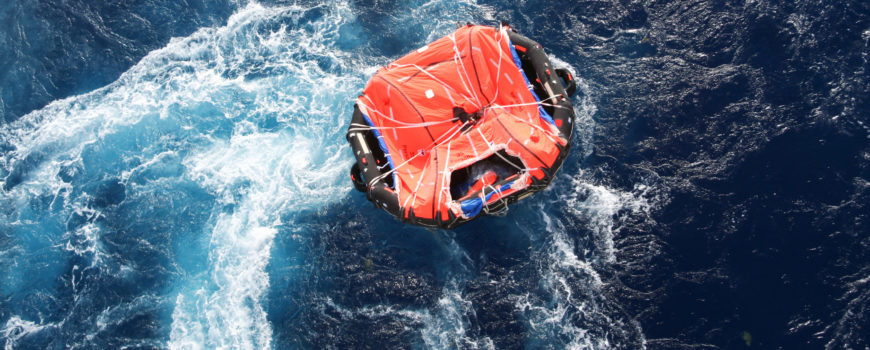
We’ve talked about clinical trial readiness repeatedly in this space. Probably we all, as an industry, have a good sense of what that means — or what it used to mean. The definition has acquired a whole new dimension in recent days. For example, this post was originally planned to be about a theoretical subset of sites that have access to plenty of patients, but are not in a sufficient state of readiness to see and treat those patients properly. Today, with a pandemic raging, the more common problem is likely to be that most non-essential patient visits have been canceled and sites are consumed with COVID-19 preparations and response.
What does “clinical trial readiness” look like then in this new world? And, what must we do to be ready to successfully operate a clinical trial today?
The fact is that any trial that will be able to continue and be successful under the current circumstances will need to have a significant virtual component. That’s one consideration, and the shift to virtual trials has been discussed by many in recent days, but there are other implications that must be addressed: The standard of care is rapidly changing. Supply chains are slowed or blocked. Patients may not be able to receive shipments of investigational product. There are also education, safety, monitoring, and data reporting challenges to resolve.
You and your team and your sites must change accordingly to meet each of these challenges.
Things You Need to Know
How do you prepare and evaluate the readiness of your teams, your sites, and your patients to move forward under this new model?
- If a trial is underway, should you pause it? Speed it up? Shut it down?
- Which of your sites will be able to move forward and which won’t?
- Which procedures can be accomplished at home or by call centers and how do you quickly prepare the staff to ensure patient safety and minimize missing data?
- How do you prepare team members to take on new roles and acquire necessary new skills?
- What patient education is necessary to ensure patients’ safety in this new paradigm?
How can you get the answers to these important questions? We can assist you with that.
The Ways in Which We Can Help
Like many of our colleagues across the industry, our team at ArcheMedX has been working overtime to develop the tools researchers and healthcare providers need to continue moving their work forward in these challenging times.
- We have made our platform available to healthcare and life science partners to deliver COVID-19 related education and training free of charge (Learn more about the offer here).
- We have collaborated with the Johns Hopkins School of Medicine, DKBMed, the Post Graduate Institute of Medical Education, and FreeCME to develop and distribute our first COVID-19 education and training experience to frontline healthcare workers (Access this free education here).
- And, we are rapidly preparing new solutions to address today’s acute readiness challenges.
In the coming days, we will release a Rapid Readiness Assessment offering, a tool designed to quickly give you the answers to how prepared your staff, sites, and patients really are to safely conduct a study in this challenging environment.
What You Can Do Right Now
In the meanwhile, know that there is already a great deal ArcheMedX can offer you in terms of identifying the important strengths and critical weaknesses of your staff and trial sites. If you would like to discuss your particular situation, we invite you to schedule a free, no-obligation consultation with a member of our senior leadership team.
As always, we are here and committed to helping.





 We recently talked with Mike Keens, Chief Operating Officer at Firma Clinical Research, a clinical research service provider specializing in patient-focused trial designs, often with at-home visit support. We wanted to share these excerpts from the conversation:
We recently talked with Mike Keens, Chief Operating Officer at Firma Clinical Research, a clinical research service provider specializing in patient-focused trial designs, often with at-home visit support. We wanted to share these excerpts from the conversation: